Managing symptoms
Nutrition to help manage PMDD symptoms
Irritability, fatigue and food cravings can affect women with PMDD. Skipping a meal will cause blood sugar to fall. This is likely to worsen irritability, fatigue and food cravings.
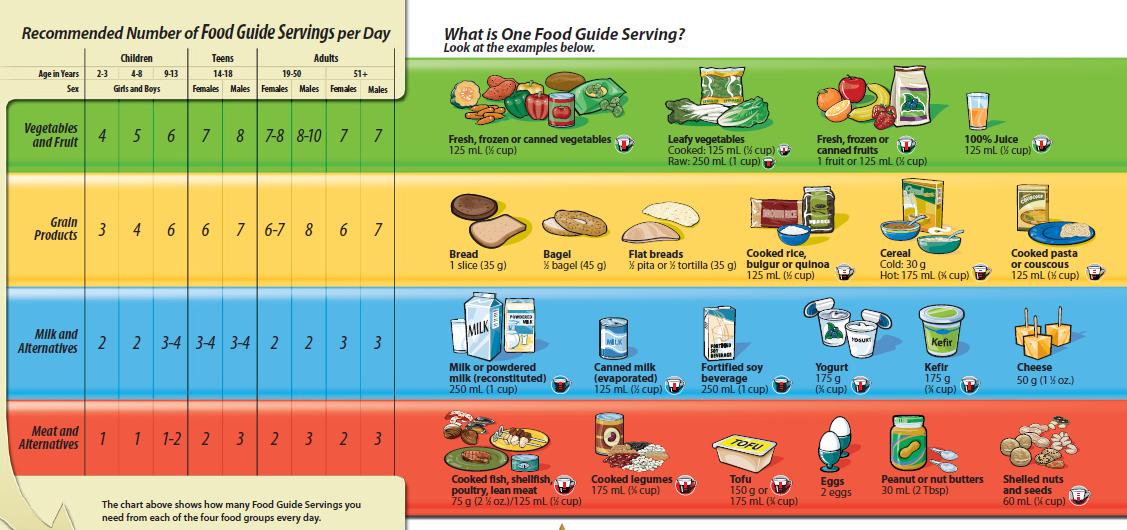
To maintain a stable blood sugar eating has to take place at regular intervals. Breakfast should be eaten soon after waking up. There should be no more than about 4 hours between breakfast and lunch and between lunch and the next meal or snack.
Plan meals including something from 3 or more food groups. Including meat and alternatives or milk products will provide protein. Protein slows the passage of food from the stomach to intestine helping to control hunger signals and stabilize blood sugar.
Drinking coffee and tea if you have PMDD
Caffeine can increase irritability and anxiety and affect sleep. Women with PMDD vary in how much caffeine they can tolerate. Some find they need to avoid coffee, tea and other caffeinated drinks altogether in the days leading up to menstruation. Other women find just cutting down on their usual intake helpful.
Total your caffeine consumption for a typical day. Does it exceed 200 mg? If so, make a plan to decrease it to 200mg per day or less if you are affected by 200mg per day. Do this over a few weeks to avoid withdrawal symptoms such as fatigue and headaches.
Source | Caffeine (mg) | Servings per day | Total (mg) Caffeine |
| Coffee (250 ml or 8 oz) | 95 | __ | __ |
Tea (250 ml or 8 oz) | 50 | __ | __ |
Iced or green tea (250 ml or 8 oz) | 30 | __ | __ |
Pop with caffeine (280 ml or 10 oz) | 35-50 | __ | __ |
Hot chocolate from mix (250 ml or 8 oz) | 25 | __ | __ |
Dark chocolate bar (56 g or 2 oz) | 45 | __ | __ |
Using alcohol with PMDD
Women with PMDD should be careful about using alcohol. It is a depressant meaning it may worsen depressed mood. It is not a good option for controlling stress.
Nutrient or herbal supplements to manage PMDD symptoms
Check out the following chart for research findings and safety considerations on supplements. Note: Unless a supplement has an NPN (natural product number), the government has not checked it to make sure it's pure and provides what it says.
Although still controversial, some research suggests that omega 3 oil from fish may be beneficial in those with depression.
The American Psychiatric Association advises that all adults eat fish at least twice a week. For those with mood disorders, they also recommend >1 g/day of EPA and DHA combined. For some patients medication will also be required.
Safety considerations
Taking too much may increase bleeding time if a cut occurs. Up to 3 grams/day (EPA+DHA combined) is considered safe by the US FDA.
Those using diabetes or blood thinning medication or supplements of garlic, gingko biloba or vitamin E may need to be more cautious; these can increase tendency to bleed.
To ensure a pure supplement, look for 'NPN' or 'IFOS' (International Fish Oil Standards) or 'molecularly distilled' on supplement labels.
A large study on women free of PMS that observed calcium intakes for 10 years found that women with an average intake of 1200 mg calcium vs 500 mg calcium were 30% less likely to develop PMS.
Two double blind trials had women with PMS take 1000-1200mg calcium daily and placebo, each for 3 menstrual cycles. By the second or third cycle, PMS symptoms improved with both treatments, but more so with calcium.
1000-1200 mg daily is prudent. 2.5-3 choices from the "Milk & Alternatives" group with a varied diet will provide this. If food sensitivities prevent this, get help from a dietitian.
Safety considerations
Going beyond 1200 mg/day through food is not a concern but through supplements could be a concern. Stomach upset, constipation and interference with absorption of other minerals are possible side effects.
An adequate vitamin D intake (600 IU/day) is important for bone health. It may also have a positive effect on mood, but more research is needed. A large group of women without PMS were studied for 10 years. Those getting an average of 700 IU vitamin D/day were about 40% less likely to get PMS than those getting an average of 100 IU/day.
This doesn't mean that vitamin D prevents PMS, but it does support meeting the recommended intake of 600 IU/day.
Safety considerations
The Institute of Medicine (Canada & US governments) that sets guidelines for vitamin D advise not exceeding 4000 IU/day.
Magnesium is controversial. While some studies have not found an effect, one small study comparing 360 mg magnesium to placebo found a beneficial effect on PMS symptoms after 2 months.
Safety considerations
Taking more than 400mg/day may cause loose stools or diarrhea.
Supplements are controversial. They can act like drugs in the body and are not always well researched. Before taking an herbal supplement, check in with your GP or psychiatrist
Other self-care tips for mild to moderate PMDD
Reduce stress. Symptoms can worsen when you are under stress so use stress-reduction strategies, such as well-balanced diet, adequate sleep, and regular exercise.
Rest and relaxation. Sleep is a priority. The brain biochemistry resets itself during sleep. Two chemicals in particular are important in this process: melatonin and oxytocin. Melatonin is released by the pineal gland in the centre of the brain. Melatonin helps you maintain your regular sleep cycle. Oxytocin is a hormone that triggers the let down of breast-milk, promotes the contraction of the uterus during menstruation and in labour, and resets the chemicals in the brain.
- Increases the level of endorphins - the body's mood-enhancing substances
- Energizes you and reduces jitteriness
- Increases levels of serotonin and dopamine in the brain, therefore helping your brain to regulate itself
- Increases your ability to deal with daily stressors
- May diminish premenstrual symptoms and depression in some women
Treating severe PMMD
Some women with severe PMDD find that self-care measures are not enough and the physician may recommend medication.
The latest research indicates that serotonin dysregulation is involved in PMDD. Women with severe PMDD symptoms can be treated with serotonin-reuptake inhibitors or SSRIs, such as Prozac, Zoloft, Luvox, Paxil and Anafranil. The SSRI medications work by increasing the amount of serotonin available to the brain - the SSRIs hold the amount of serotonin in the brain stable even as the woman's hormones fluctuate.
When serotonin medications cannot be tolerated, a different type of antidepressant called Effexor is an alternative. It enhances serotonin levels and balances the norepinephrine pathways.
Each woman reacts differently to medications. Therefore, women are encouraged to talk to their doctor about the medication and possible side effects.
Some women may need medication only for the last two weeks of their menstrual cycle, while other women may need to take medication daily to alleviate their symptoms. SSRIs will not effect your normal menstrual cycle.
Medications do not stop symptoms immediately. It may take several weeks or months for the proper blood levels to be established so the SSRIs can have the maximum effects.
Research shows that progesterone had absolutely no effect on PMDD symptoms. For some women who are anxious, irritable and restless, progesterone may bring some relief.
More research is needed on the use of estrogen for PMDD. However, for most women with PMDD, long term estrogen use is not appropriate because of side effects such as over-stimulation of uterine lining and heavy bleeding.
The ultimate goal is to utilize the appropriate self-care and medication strategies with each woman experiencing PMDD.